Back Pain
Intervertebral Disk (IVD)
Disc-related injuries are most commonly associated with the lowest part of our spine (L4-S1) and the base of our necks (C5-T1). This is because they are two of the most mobile areas of the spine and the discs are more likely to undergo a wider range of stress. Degenerative discs are a common finding using MRI scans, even in patients with no pain, and they are often found at these areas too.
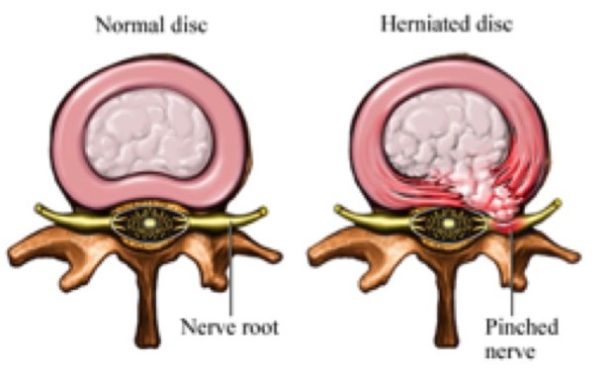
But a disc injury is not an ‘on and off’ injury and has a range of presentations, physically and symptomatically. The picture indicates normal and ‘worst case’ scenario discs, whereby the jelly-like core of the disc (a.k.a the nucleus pulposus) pushes through damaged or strained outer fibers (a.k.a the annulus fibrosus).
A ‘disc prolapse’ can be anywhere along this spectrum*, from a mild bulge to full herniation, which can cause stenosis (narrowing of spinal canal) which can potentially compress nerve roots or sciatica**.
Common symptoms may include lower back pain, pain radiating into the back of the thigh, calve and/or foot, pins and needles, numbness and/or weakness in the upper and/or lower limb(s). Additional sequalae, such as altered bladder and/or bowel function, should prompt immediate medical referral.
Treatment Plan:
Every patient is unique and the approach will reflect this. Together, you and your osteopath will discuss a course of action and treatment which best suits you. Common key areas to be addressed may include:
- Local musculature – appropriate strength, stamina and suppleness of gluteals, iliopsoas, erector spinae, abdominals, quadriceps, hamstrings and piriformis
- Spinal joint function – at site of injury as well as above and below
- Pelvic and hip joint function – sacroiliac joints and symphysis pubis
- Rib function and breathing mechanics
- Bowel function – repetitive straining increases intra-abdominal pressure
- Stress
* Fandon et al. 2014. Lumbar disc nomenclature: version 2.0 The Spine J. 14(11): 2525–2545
**Nice. 2017. Sciatica (lumbar radiculopathy) Available at: https://cks.nice.org.uk/sciatica-lumbar-radiculopathy#!backgroundsub:2 [Accessed on 14/06/2017]
Muscle spasm/tightness & Joints
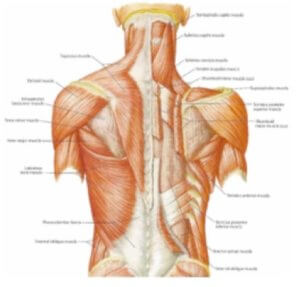
The major muscles of the back are depicted in the graphic including the erector spinae, the gluteals, trapezius and latissimus dorsi.
The joints of the back are in pairs on either side of the spine. They include the facet joints (between spinal bones), the costovertebral and costotransverse joints (between rib and spinal bones) and at the base of the spine the sacroiliac joints where the sacrum articulates with the pelvis.
Any of these joints have the potential to become over stressed, restricted or irritated which could be reflected in the muscles overlying it.
The most common causes of back pain are the three usual suspects: joint, muscle and disc; or a combination of any or all of these. Back pain will, in most cases, involve a muscular element but with an intricate relationship with its surrounding structures.
Typical symptoms may include:
- Localised pain/spasm +/- tenderness on palpation
- Sudden onset especially after injury or repetitive use
- Morning stiffness/ reduced mobility
- Referral pain from a muscle to a distal location
- Weakness/ pain with movement
Treatment Plan:
Every patient is unique and the approach will reflect this. Together, you and your osteopath will discuss a course of action and treatment which best suits you. Common key areas to be addressed may include:
- Local musculature – appropriate strength, stamina and suppleness of gluteals, iliopsoas, erector spinae, abdominals, quadriceps, hamstrings and piriformis
- Influence of any joint dysfunction – facets, costovertebral and costotransverse.
- Shoulder and hip dysfunction – attributing to compensatory patterns
- General exercises and mobility
- Effects of ergonomics, posture and work-related activity on pain
Bone
Throughout our lives our bones form, deform and re-form. They are a constantly changing and adapting to the forces put through them (walking, running, jumping, gravity etc) and not merely a dead structure that our muscles attach to.
Unfortunately, our bones and joints can fail or maladapt which can create problems such as:
- Spondylarthrosis/ Spondylosis – where the facet joint cartilage and/or discs wear over time and can cause restricted movement and sometimes pain
- Osteoporosis/ Osteopenia – reduced bone mineral density which can predispose us to fractures. This is significantly predisposed by external factors such as diet, hormones, steroid medication and physical activity
- Scoliosis – a deviation from the normal curvatures of the spine which can impact quality of life and organ functionality depending on severity
- Inflammatory arthropathy – immune system-related malfunction which affects the soft tissues and joints causing stiffness, pain and joint damage e.g. rheumatoid arthritis, ankylosing spondylitis and psoriatic arthritis
- Spondylolisthesis/ fractures – different areas of the spine can fracture which creates pain, dysfunction and/or spinal cord compression
- Cancer/ Metastasis – the spine is a common sight for cancer to develop or travel to from other organs affected by cancer
Treatment plan: Each of the above would need a different treatment and management plan but would include:
- Diet assessment – checking that you are getting the appropriate amount and types of food to prevent exacerbation of the condition
- Mobility assessment – creating movement where restricted or impeded
- Exercise and lifestyle advice
- Support and Reassurance
If fractures, inflammatory arthropathy or cancers are suspected by your osteopath, referral to your GP for further investigations and management would be discussed with you.
Postural compensations/Adaptations
Posture is a hot topic and is often brought up when discussing back pain, amongst other things.
But how important is posture on our individual problems?
Standing, sitting, walking, sleeping – all are different postures and exert different stresses. We can all relate to when one of these positions became uncomfortable. But why? Posture is an adaptive dynamic positioning of our body to allow it to function effectively and easily with the stress that is put upon it.
The reason we get aches and pains with ‘poor posture’ is because we have lost conscious awareness of our body positioning, and the joints, muscles and ligaments are put into a single position for too long. Poor posture is habitual positioning that puts unnecessary strain through our bodies.
It is the lack of movement that is important to consider in these straining positions. Even having a perfect posture without movement or regular changes in position could be just as stressful on our bodies.
Treatment plan: correcting posture is long and demanding and requires active engagement if it is something that truly needs ‘correcting’. Often our posture is one element of a bigger picture which may be attributing to your pain or problem. The main focuses of treatment are:
- Creating body awareness – knowing when to change from a ‘habitually straining’ position to a more neutral less stressful position
- Encouraging movement breaks – find an accused to move around and get out of one position – go outside for fresh air, make a cup of tea, get a drink, go to the printer, talk to a colleague rather than email.
- Seated exercises to introduce movement, relieve stiffness and promote body awareness
- Ergonomics – making your workspace/bed/gait more appropriate/supportive for your body
- Pain – treating areas of discomfort that could be facilitating the poor posture, also known as an antalgic (avoiding pain) posture
- Strength, Suppleness and Stamina training – our muscles and joints need to be conditioned to cope with the stresses you put upon it, this includes the posture we adopt
*Painscience. 2017. Does posture correction matter? Available at: https://www.painscience.com/articles/posture.php [Accessed on 14/07/2017]
**Lomas-Vega et al. 2017. Effectiveness of Global Postural Re-education for Treatment of Spinal Disorders: A Meta-analysis. Am J Phys Med Rehabil. 96(2):124-130


