Hip Pain
The Hip and Pelvic Joints
The hip is the articulation of the ball of the femur with the socket of the pelvis. Like the shoulder, it is a ball and socket joint with a wide range of motion. However, the hip is very stable as part of its weight bearing role thanks to the depth of the socket and powerful surrounding capsule, ligaments and muscles.
The pelvis is made up of two innominate bones which articulate at the pubis (pubic bone) at the front and to the sacrum at the back. This forms a pair of sacroiliac joints with even stronger ligaments and fine motion which aid in the normal gait (walking) cycle allowing ground forces to disperse from the feet to the spine and beyond.
The following list is by no means exhaustive but aims to cover and explain the most common disorders and problems we see in clinic.
Hip Osteoarthritis (OA)
Commonly affects the ‘elderly’ and as with all types of osteoarthritis (OA), it is a disease caused by overuse, misuse, disuse or a combination of. The upper part of the ball of the femur is the main weight bearing part of the joint and tends to be where the ‘wear and tear’ starts. The robust hyaline cartilage that pads the joint can start to thin out causing irritation of more sensitive structure beneath (synovium and subchondral bone).
Typical Symptoms may include:
- Insidious onset
- Relieved by rest
- Stiffness or restricted hip movement
- Difficulty walking/ going up and down stairs
- Change in walking style
- Pain in the groin, buttock, thigh or knee
- Pain can be sharp, stabbing or a dull ache
Treatment plan: Osteoarthritis cannot be cured with osteopathy; however, we can manage and relieve the discomfort/pain you may be suffering from. Together, you and your osteopath will discuss a course of action and treatment which best suits you. Common key areas to be addressed may include:
- Lower limb biomechanics – identifying and treating any compensatory patterns of the feet, ankles, knees and hips that may aggravate symptoms
- Local muscle function and tone – weakness of the gluteals (buttocks) can lead to poor hip function and control. Other muscles to consider include the adductors, hamstrings, quadriceps and lumbar spine musculature
- Pelvis and Lumbar spine function and mobility
- Activity and Exercise – retraining the hip and surrounding areas
- Nutritional support
- Further afield – thoracic spine and diaphragm
- Confidence and support with movement
- Referral to orthopaedics for further investigations if necessary
- Is surgery an option for you?
Labral Tear
The socket of the hip (acetabulum) is surrounded by a thick hyaline cartilage known as the labrum. The labrum provides support and stability to the hip joint. The labrum can tear due to impingement (bony impaction) of the femur on the acetabulum, repeated use in sport or activity or sometimes for no particular reason.
Typical Symptoms may include:
- Pain in the groin, hip or buttock
- Catching or clicking with hip movement
- Reduced hip mobility
- Pain on deep squatting or weight bearing
- Hip giving way
Treatment plan: Every patient is unique and the approach will reflect this. Together, you and your osteopath will discuss a course of action and treatment which best suits you. Common key areas to be addressed may include:
- Avoid/reduce aggravating factors – such as seated positions, activity and sport
- Assess biomechanics of the hip, pelvis and spine – address any problems
- Spinal mechanics – appropriate spinal mobility is important in the gait (walking) cycle.
- Restrictions could be attributing to poor gait mechanics
- Local musculature – tight hip flexors (iliopsoas, quadriceps, adductors) or weak external rotators (gluteal medius, piriformis) could occur as a consequence of a labral tear
- Strengthening and proprioception – engaging weakened muscles, improving balance and creating confidence in movement
- Graded return to normal physical activity
- Referral to orthopaedics for further investigations if necessary/ discuss options for surgery (depending on severity)
Greater Trochanteric Pain Syndrome a.k.a Trochanteric Bursitis
Bursitis is a term to describe an inflamed bursa. Bursas are fluid-filled sacs that are found throughout the body to reduce friction as muscles/tendons move against bony prominences. The greater trochanter is the superficial bony area of the hip. The main bursa believed to be involved in this condition is that which resides over the greater trochanter.
Bursitis is believed to be caused by repetitive or acute trauma, repetitive movements, sporting injury or unfamiliar strenuous exercise.
Studies have demonstrated that more than just the greater trochanteric bursa may be involved in this painful condition. These include gluteal muscle myofascial trigger points (MFTPs), tendinopathy, lumbar spine or hip pathology, ITB disorders and/or other surrounding tissues. Hence now known as Greater Trochanteric Pain Syndrome (GTPS) to account for all the possible causes of the pain.
Typical Symptoms may include:
- Pain over the outer part of your hip
- Pain may radiate to the outside of the knee or buttocks
- Aggravated when lying on the affected side, especially at night
- Gradual or traumatic onset
- Aggravated by overuse
- Difficulty climbing stairs or standing from a seated position
Treatment plan: Every patient is unique and the approach will reflect this. GTPS can be complex due to the over-lapping of causes and symptoms. Together, you and your osteopath will discuss a course of action and treatment which best suits you. Common key areas to be addressed may include:
- The cause of the ‘bursitis’ – bursitis is a symptom of the problem and may be caused by over working overlying muscles, malfunctioning hip/pelvis/spine biomechanics or a combination of these.
- Treat any associated disorders – MFTPs of surrounding musculature, hip, lumbar spine and pelvic pathology.
- Gait (walking) style
- Sleeping and sitting ergonomics
- Pain management – hydrotherapy, stretching and/or pain killers
- Surgical options are rarely indicated
Sacroiliac Joint Dysfunction
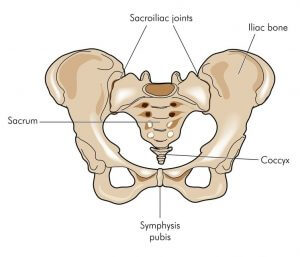
The sacroiliac (SI) joint is the articulation between the sacrum of the spine and the ilium of the pelvis. It is a very stable joint with subtle movement for appropriate gait (walking) mechanics which allows for integrated motion through the hip, pelvis and spine.
The surrounding ligaments are some of the strongest ligaments in the body and, with the contours of the bones and dynamic muscle stabilisers, creates the very stable, but mobile, SI joint.
Dysfunction of the SI joint can occur either from direct trauma, repetitive excessive loading, hypermobility (too much) or hypomobility (too little). This can mimic other causes of lower back pain as symptoms overlap.
Typical Symptoms may include:
- Lower back pain – dull, sharp, stabbing
- Pain into the buttock, thigh or calve
- Painful to lie on affected side
- Aggravated with hip movement and sitting
- Associated with recent/current pregnancy
- Possible pins and needles or numbness
The SI joint is commonly involved with inflammatory disorders such as Ankylosing Spondylitis, Reactive Arthritis and Rheumatoid Arthritis. These must be treated in a multi-disciplinary fashion involving your osteopath, GP and rheumatologist.
Treatment plan: Every patient is unique and the approach will reflect this. Together, you and your osteopath will discuss a course of action and treatment which best suits you. Common key areas to be addressed may include:
- Hypermobile joint or flexibility in a hypomobile joint – exercises and mobilisation to improve this
- Lumbar spine and hip dysfunction – the lower lumbar spine is intimately related to the SI joints and would need to be assessed and treated as appropriate
- Deep muscle stabilisers such as piriformis, quadratus femoris, obturators and gemelli
- Other local musculature – adductors, gluteals, hamstrings and quadriceps
- Gait analysis – gluteal weakness, hip, knee and ankle biomechanics
- Systemic causes – exclude underlying causes such as inflammatory disorders, infection, bowel related disease
Piriformis Syndrome
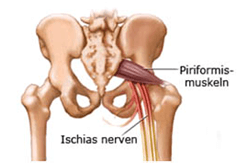
The piriformis is a muscle that runs between the sacrum to the femur bone. It allows for external rotation and abduction movement. The sciatic nerve, the main nerve the innervates the majority of the leg and thigh muscles and skin, is in close proximity to the piriformis and sometimes can penetrate through the muscle itself.
Piriformis Syndrome is whereby the piriformis muscle has become overly tight due to spasm or contracture which creates pressure on the underlying sciatic nerve. This causes irritation/compression of the nerve (neuritis) which creates sciatica-type symptoms. This diagnosis is still controversial1 but creates an understanding to work from and treat.
Typical symptoms may include:
- Ongoing/ long term pain in the buttocks and/or lower back
- Pain radiating into the back of the thigh, calve and/or foot
- Pins and needles, numbness or weakness in the leg or foot
- Aggravated by straining or having a bowel motion
- Aggravated by sitting – adjust sitting position to relieve pain
- Aggravated by moving hip inward
- Dyspareunia in women (painful intercourse) – uncommon
- Pain around genitalia – uncommon
Treatment plan: Every patient is unique and the approach will reflect this. Together, you and your osteopath will discuss a course of action and treatment which best suits you. Common key areas to be addressed may include:
- Pain management – pain killers, hydrotherapy etc
- Piriformis muscle tightness or myofascial trigger points (MTFPs) – stretches, mobility exercises and direct treatment
- Pelvic floor muscle dysfunction/weakness
- Sacroiliac joint, lumbar spine and hip dysfunction
- Sitting and sleeping ergonomics – that may be attributing to the problem
- Nerve mechanics – assess and treat sciatic nerve mobility
1.Hopayian et al. 2010. The clinical features of the piriformis syndrome: a systematic review. Eur Spine J. 19(12): 2095-2109


