Neck Pain
Intervertebral Disk (IVD)
Disc-related injuries are most commonly associated with the lowest part of our spine (L4-S1) and the base of our necks (C5-T1). This is because they are two of the most mobile areas of the spine and the discs are more likely to undergo a wider range of stress. Degenerative discs are a common finding using MRI scans, even in patients with no pain, and they are often found at these areas too.
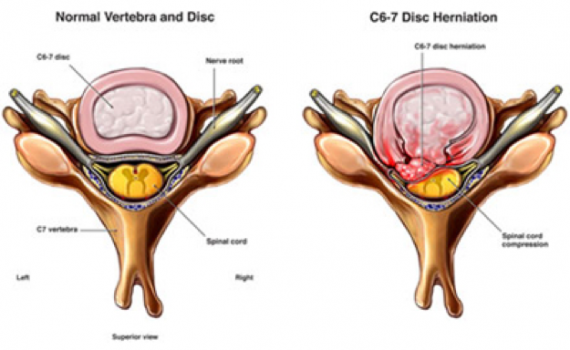
But a disc injury is not an ‘on and off’ injury and has a range of presentations, physically and symptomatically. The picture indicates normal and ‘worst case’ scenario discs, whereby the jelly-like core of the disc (a.k.a the nucleus pulposus) pushes through damaged or strained outer fibers (a.k.a the annulus fibrosus).
A ‘disc prolapse’ can be anywhere along this spectrum1, from a mild bulge to full herniation, which can cause stenosis (narrowing of spinal canal) which can potentially compress nerve roots2 (see Nerve Impingement).
Common symptoms may include neck pain, headaches, difficulty moving the head, pain radiating into the shoulder, arm and/or hands, pain radiating into the lower limb(s), pins and needles, numbness and/or weakness in the upper and/or lower limb(s). Additional sequalae, such as altered bladder and/or bowel function, should prompt immediate medical referral.
Treatment Plan: Every patient is unique and the approach will reflect this. Together, you and your osteopath will discuss a course of action and treatment which best suits you. Common key areas to be addressed may include:
- Local musculature – appropriate strength, stamina and suppleness of trapezius, levator scapulae,
- cervical erector spinae, semispinalis, splenius capitis, suboccipitals and muscles related to the
- shoulder blade.
- Spinal joint function – at site of injury as well as above and below
- Shoulder girdle function – scapulothoracic, glenohumeral and acromioclavicular joints
- Rib function and breathing mechanics
- Head, neck and shoulder posture
- Stress
- GP/Orthopaedic referral for scans, only if necessary
1.Fandon et al. 2014. Lumbar disc nomenclature: version 2.0 The Spine J. 14(11): 2525–2545.
2.Nice. 2017. Sciatica (lumbar radiculopathy) Available at: https://cks.nice.org.uk/sciatica-lumbar-radiculopathy#!backgroundsub:2 [Accessed on 14/06/2017]
Nerve Impingement
Our brain and spinal cord makes up the Central Nervous System (CNS) and is protected by the bony arrangements of our skull and spine. The peripheral nervous system (PNS) is an extension of the CNS and comprises the nerves that innervate the organs, muscles and the major sensory organ, the skin.
Nerve impingement, or compression, is where-by the nerve root (the part of the nerve exiting the spine) is encroached by local structures in the neck such as discs, cysts or bony changes. This can create radiating pain into the neck and upper limb known as Cervical Radiculopathy1.
Other symptoms may include:
- Local muscular spasm in the neck
- Aggravated by neck motion, especially looking down
- Weakness in the arm or hand
- Pins and needles/ change in sensation/ numbness in the arm or hand
Treatment plan: The cause of your cervical radiculopathy will dictate the type of treatment that is appropriate for you. Together, you and your osteopath will discuss a course of action and treatment which best suits you and your unique problem. Common key areas to be addressed may include:
- Local musculature – appropriate strength, stamina and suppleness of trapezius, levator scapulae, cervical erector spinae, semispinalis, splenius capitis, suboccipitals and muscles related to the shoulder blade.
- Spinal joint function – at site of injury as well as above and below
- Shoulder girdle function – scapulothoracic, glenohumeral and acromioclavicular joints
- Rib function and breathing mechanics
- Head, neck and shoulder posture at work, at home and on the move
- Stress
- GP/Orthopaedic referral for scans, only if necessary
1.Medscape 2016. Cervical Radiculopathy. Available at: http://emedicine.medscape.com/article/94118-overview [Accessed on 14/06/2017]
Muscles & Joints
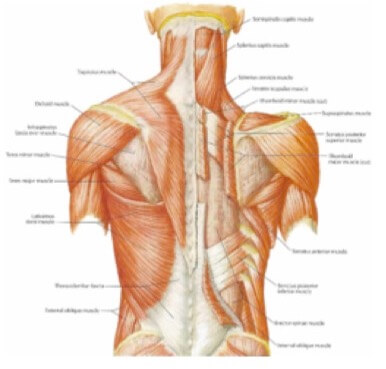
There are several layers of muscles of the neck in the back, front and sides. The major muscles include the scalenes, trapezius, splenius capitis and sternocleidomastoid. The deep muscles of the front of the neck are involved with swallowing.
As a continuation of the whole spine, the joints of the neck are in pairs like that of the rest of the spine. These are called facet joints and allow the vertebrae to glide to allow movement.
These joints have the potential to become over stressed, restricted or irritated which could be reflected in the muscles overlying it.
The most common causes of neck pain are the three usual suspects: joint, muscle and disc; or a combination of any or all of these. Neck pain will, in most cases, involve a muscular element but with an intricate relationship with its surrounding structures.
Typical symptoms may include:
- Localised pain/spasm +/- tenderness on palpation
- Sudden onset especially after injury, awkward sleeping position or repetitive use
- Morning stiffness/ reduced mobility
- Referral pain from a muscle to a distal location
- Weakness/ pain with movement
Treatment plan: Every patient is unique and the approach will reflect this. Together, you and your osteopath will discuss a course of action and treatment which best suits you. Common key areas to be addressed may include:
- Local musculature – appropriate strength, stamina and suppleness of trapezius, levator scapulae, cervical erector spinae, semispinalis, splenius capitis, suboccipitals and muscles related to the shoulder blade.
- Facet joints – Influence of any joint dysfunction in the neck
- Upper rib/breathing dysfunction
- Shoulder and hip dysfunction – attributing to compensatory patterns
- General exercises and mobility
- Effects of ergonomics (desk, sleeping, driving), posture and work-related activity on pain
Headaches

There are several different headaches each with a slightly different presentation, cause and treatment. Common examples include:
Tension headaches are related to neck and head muscle tension which refers pain to the head. Most commonly present with a band-distribution around the head, across the forehead or over one eye.
Cervicogenic headaches are more complex and are believed to be an interaction between the nerves leaving the trigeminocervical nucleus in the brain stem, the cervical (neck) spinal nerves and spinal accessory nerve1. It can present with neck stiffness, neck pain, face pain and neck tenderness.
Migraines are described as a ‘complex condition with a variety of symptoms…. Painful throbbing one-sided headache, disturbed vision, sensitivity to light and sound, nausea and vomiting2. There is no known cure and we don’t fully understand why they happen but genetic and environmental components are involved. Migraines tend to have environmental triggers such as: alcohol, stress, lack of food, certain types of food, lack of sleep and hormonal changes2.
Headaches need to be assessed and treated appropriately to ensure no sinister underlying cause but fortunately they tend to fall into one or a mix of the above primary types. Secondary headaches are those headaches that are a consequence of something else including trauma, infection, dental pain, medication or dehydration.
Treatment plan: Every patient is unique and the approach will reflect this. Together, you and your osteopath will discuss a course of action and treatment which best suits you. Common key areas to be addressed may include:
- Local musculature – identification and treatment of myofascial trigger points (MFTP) of the head, neck and shoulders.
- Facet joints – Joint dysfunction associated with any MTFPs
- Sinus and/or jaw function – these areas may also contribute towards your headaches
- Upper rib/breathing dysfunction – attributing to further neck tension
- General exercises and mobility
- Effects of ergonomics (desk, sleeping, driving), posture and work-related activity on pain
- Identifying and modifying ‘triggers’ – foods, stress, etc.
1.Biondi, D.M. 2005. Cervicogenic headache: a review of diagnostic and treatment strategies. J Am Osteopath Assoc. 105 (16S-22S)
2.The Migraine Trust. 2017. More than ‘’just a headache’’. Available at: https://www.migrainetrust.org/about-migraine/migraine-what-is-it/more-than-just-a-headache/ [Accessed on 12.06.17]
Neck Injury / Whiplash

A cervical (neck) acceleration/deceleration injury is more commonly referred to as a whiplash injury or whiplash-associated disorder (WAD). It is a frequent complication of road traffic collisions and can last for several months. The severity of the trauma often does not correlate well with symptoms and, as such, imaging does not help with management and diagnosis is mainly based on clinical findings1.
A grading system (Quebec Taskforce on Whiplash-Associated Disorders) helps to determine the severity of the injury and management from no symptoms (0) to neck symptoms with fracture/dislocation (4)1.
The source of the pain felt in these types of injury have been theorised to be associated with straining and/or tearing of the soft tissue (muscles/ligaments) and possible further injury/irritation/compression to joints and nerves. Haemorrhaging (internal bleeding), swelling and inflammation may also occur consequently1.
Typical Symptoms may include:
- Ongoing motion-induced neck pain
- Headache (see cervicogenic headache)
- Delayed onset neck pain post-injury
- Muscle tension/guarding
- Facet joint dysfunction (associated with headaches)
- Shoulder/Arm pain
- Visual disturbances
- Tinnitus (ringing in the ear)
- Dizziness
- Concussion
- Weakness/ numbness/ pins and needles in the upper limb
- Difficulty sleeping
- Difficulty swallowing, bladder and bowel dysfunction requires immediate medical attention
Treatment plan: a multi-disciplinary approach is recommended for whiplash involving your doctor, osteopath or physiotherapist and pharmacist who can support you through your recovery. Depending on symptoms, referral to other appropriate specialists may be necessary. Common areas your osteopath would want to address may include:
- Self-care advice – return to usual activities as early as possible. Some discomfort is to be expected but is not indicative of further damage. Avoid immobilisation, collars and excessive rest
- Exercise advice – bring confidence back into your movement
- Painkillers – to moderate pain and allow for return to activity
- Psychological factors – stress, expectation, anxiety, fear, litigation issues.
- Joints and muscles – the immediate area of injury may be too tender for direct treatment. Other secondary compensation areas (shoulders, upper back, chest) may be more appropriate for treatment
1.2015. Cervical Sprain and Strain. Available at: http://emedicine.medscape.com/article/306176-overview [Accessed on 13.06.17]


